Surgery and Anti-wrinkle Injections for Facial Palsy
Facial palsy refers to a paralysis (weakness) of the facial muscles. It can either be congenital (meaning you are born with it) or acquired from a variety of causes including Bell’s palsy, Ramsey Hunt syndrome, Lyme disease, tumours or trauma among others. Regardless of the cause facial palsy can lead to
- difficulties raising the eyebrow
- difficulties closing the eyelids with potential damage to vision
- difficulties breathing through the nose
- difficulties with speech
- weakness or failure to smile with ensuing facial asymmetry
- hyperkinesis (tightness due to aberrant nerve recovery)
- synkinesis (unwanted movements due to aberrant nerve recovery)
- consequential social isolation and potential psychological issues
Mr Johnson has founded, established and has led the Oxford Facial Palsy Service since 2012. He has promoted, developed and coordinated a multidisciplinary team approach to the rehabilitative management of both children and adults with facial palsy resulting from both congenital and acquired causes.
He works closely with an oculoplastic surgical colleague, a facial therapist and a clinical psychologist to provide the best holistic approach to the management of patients with facial palsy regardless of the cause.

Rehabilitative surgery for facial palsy is aimed at
- eyebrow elevation
- eyelid closure
- static facial suspension procedures to improve appearance at rest
- dynamic (reanimation) surgery to create an active smile
Not all patients with facial palsy are suitable for surgery and a detailed consultation is required in order to determine the most appropriate procedures.
Botulinum toxin injections can be used to treat hyperkinesis and synkinesis on the affected side as well as reducing some overactivity on the unaffected side to improve facial asymmetry. These injections are given in the outpatient clinic and are repeated every 4-6 months.
Click on the links below to find out more about each of these surgical procedures:

UK or International private referrals
Please contact private secretary and practice manager:
Marcia Pillai
Tel: 07780 514777
E-mail: davidjohnson@doctors.org.uk
Treatment costs
Initial consultation
£300
The exact surgery cost will be confirmed after your consultation. This will include the hospital, surgeon and anaesthetic fees.
This procedure is available under a self-pay basis only.
Patients with facial palsy may have drooping (ptosis) of the eyebrow on the affected side. This can either be addressed by botulinum toxin injections or by undertaking a browlift procedure similar to those used for age related drooping of the eyebrows. Usually in the case of facial palsy the direct brow lift approach is the best method and this involves the placement of a scar along the length of the top aspect of the eyebrow and can be performed as either a local or general anaesthetic day case procedure.

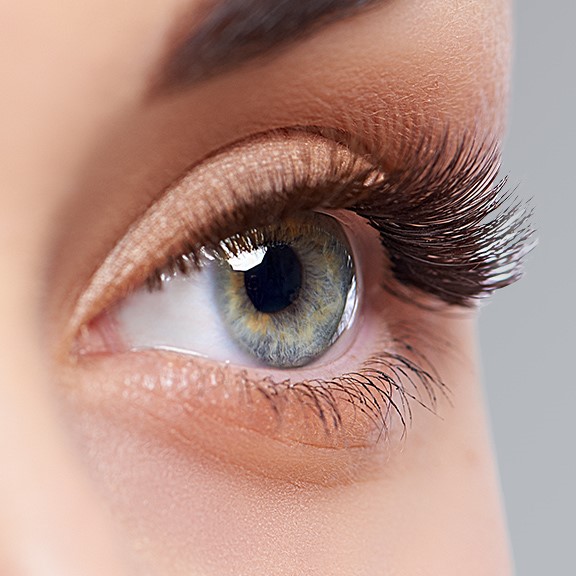
Patients with facial palsy often have problems closing their eyelids on the affected side due to a weakness of the muscle affecting both the upper and lower eyelid. This problem requires prompt treatment to prevent the cornea (front surface of the eye) from becoming too dry which, in severe untreated cases, can lead to serious and permanent damage to vision from exposure keratitis and infection. Conservative, non-surgical treatment involves using eyedrops and lubricants. In addition it may be necessary to tape the eye closed at night.
In some circumstances surgery is required and it may be beneficial to insert a weight (often made of gold or platinum) in the upper eyelid to facilitate closure of the upper lid. This leaves a small scar in the natural crease in the upper lid and is performed as either a local or a general anaesthetic day case.
If the lower eyelid is drooping or pulled away from the eyeball (called an ectropion) then this is corrected surgically by a procedure to tighten the lower lid. This leaves a small scar in the outer corner of the eyelid and is performed as either a local or a general anaesthetic day case. Often both upper and lower lid surgery are done together. Only in extreme circumstances is it necessary to either temporarily or permanently stitch the outer aspect of both upper and lower eyelids together (called a tarsorraphy procedure).
Patients with facial palsy as well as having an inability to actively smile often have drooping of the affected side of the face leading to noticeable asymmetry of the cheek and the corner of the mouth even at rest (i.e. without smiling). For a variety of reasons some such patients may not be suitable for dynamic smile surgery but could still benefit from a static procedure to lift the side of the drooping cheek. There are a number of surgical procedures that can help including a facelift or a necklift. In addition, one of the most effective procedures is to do an operation called a ‘fascial sling’ procedure. This is a general anaesthetic procedure and involves staying in hospital for one night. The operation involves making a surgical incision on the front of the thigh in order to harvest a strip of fibrous material (called fascia) on top of the muscle of the thigh. This leaves a straight line scar on the front of the thigh. Then, via an incision in the smile crease near the mouth in the lower cheek (called the nasolabial fold) together with an incision within the scalp hair of the temple region above the ear, one end of the facial strip is attached under the skin to the corner of the mouth and the upper and lower lip. The other end is then pulled tight to lift the drooped cheek/corner of the mouth and tunnelled under the skin of the cheek and attached under the scalp incision. This operation is a static procedure and so does not create an active smile but nevertheless can be very effective in improving asymmetry.

Patients with facial palsy may have weakness in their ability to smile on the affected side ranging from mild weakness to complete absence of movement. Patients with no movement at all or at lease very weak movement may benefit from dynamic smile surgery. There are number of potentially suitable procedures and I have listed the common ones I undertake here:
Sliding Temporalis Myoplasty
This operation has the benefit of being a single stage procedure. It is a particularly good option for adults over the age of 50 and for those who are not suitable for other types of procedure such as the 2 stage procedure (mentioned below). It involves a general anaesthetic and a 2 night stay in hospital. An incision is made in a zig zag shape across the top of the scalp within the hair from ear to ear as well as an incision in the lower cheek crease near the mouth (called the nasolabial fold). This provides access to one of the chewing muscles (called the temporalis muscle) which normally helps bite your teeth together. This muscle is freed from its normal bony attachments and the lower end is then stitched under the skin to the corner of the mouth and the upper and lower lip. Contraction of the muscle is instigated by biting the teeth together which now pulls on the cheek and corner of the mouth to create a smile movement. With time it may be possible to learn how to use the new muscle to create a voluntary smile without the need to bite the teeth together.
2 stage facial reanimation using a cross facial nerve graft and free muscle transfer
This technique is performed in 2 stages with each operation performed approximately 1 year apart. This is a particularly good option for young children over the age of 5 and for adults under the age of 50.
Stage 1:
The first operation is called a ‘stage 1 cross facial sural nerve graft’ and is a general anaesthetic procedure and involves a 2 night stay in hospital. During this first stage procedure a cut (incision) is made on the back of the lower leg from the knee to the outer aspect of the ankle and a nerve (called the sural nerve, which supplies sensation (feeling) to the outer aspect of the foot) is removed from the leg. This results in some minor numbness on the outer aspect of the foot but does not cause any problems with movement or balance. During the same anaesthetic a cut (incision) is made in front of the ear and extending into a natural crease line in the neck on the unaffected side of the face. This allows surgical access to the facial nerve branches so that one of the many small branches of the facial nerve causing the smile can be identified. One of these nerve branches can then be cut (without causing any weakness on the unaffected side of the face) and joined to one end of the sural nerve graft from the leg which is now transplanted into the face. The transplanted sural nerve is tunnelled under the skin of the face to a position in front of the ear on the paralysed side of the face using a small cut (incision) inside the nostril and a small cut in front of the ear on the paralysed side of the face. The nerve from the cut facial nerve branch then grows along the transplanted sural nerve graft at a rate of approximately 1 mm per day and so it takes many months for the nerve fibres to reach the other end of the nerve graft. This stage 1 operation does not in itself cause any facial movement but is necessary to set everything up for the stage 2 procedure.
Stage 2:
The second operation is called a ‘stage 2 free muscle transfer’ and is a general anaesthetic procedure and involves a 5-7 night stay in hospital. During this second stage procedure a cut (incision) is made in the inner aspect of the thigh from the region of the groin to the inner aspect of the knee and a muscle called the gracilis muscle is harvested (removed) together with its blood vessels (an artery and a vein) and nerve supply. This results in a scar on the inner aspect of the thigh but does not cause any problems with movement or balance. During the same anaesthetic a cut (incision) is made in front of the ear and extending into a natural crease line in the neck on the affected, palsy side of the face. This allows surgical access to identify the end of the previously transplanted cross facial sural nerve graft. One end of the transplanted gracilis muscle is stitched under the skin to the corner of the mouth and the upper and lower lip. The other end of the transplanted muscle is stitched under the skin to an area in front of the ear and the temple region. The nerve to the muscle is then joined to the end of the previously transplanted sural nerve graft and the transplanted blood vessels to the muscle are joined to blood vessels in the face in order to restore blood flow to the muscle and so keep the transplanted muscle alive. The nerve grows into the transplanted muscle at the rate of 1mm per day and so it can take up to 6 months to see the transplanted muscle create a smile.
The benefit of this 2 stage procedure is that the movement of the transplanted muscle is synchronised with the muscles of the opposite unaffected side and so no voluntary thought is required to instigate the movement thus providing the possibility of spontaneous laughter.
Nerve transfers
If the facial muscles have not been stimulated by the facial nerve for 2 years then these muscles will no longer be able to work normally. The ability for the muscles to be reinnervated is therefore less than 2 years. In certain circumstances when the facial palsy, for whatever cause, has not shown any signs of recovery whatsoever after approximately 9 months it may be appropriate to consider a nerve transfer procedure before such times that the facial smile muscles can’t recover. That way this will avoid a muscle transfer.
One such nerve transfer involves joining the nerve to the masseter muscle (one of the chewing muscles which helps you bite your teeth together) to a branch of the facial nerve on the same side as the paralysis responsible for the smile. This is a general anaesthetic procedure and requires 1-2 night stay in hospital.
During the procedure a cut (incision) is made in front of the ear and extending into a natural crease line in the neck on the affected side of the face. This allows surgical access to the nerve to the masseter muscle as well as to the non functioning facial nerve branch that should be responsible for causing a smile. The nerve to the masseter muscle is then cut (without causing any weakness of chewing on the affected side of the face) and joined to the non functioning facial nerve branch. The nerve to masseter muscle then has to grow down the facial nerve branch at a rate of approximately 1mm a day and so it can take over 3 months to see any results. Instigation of the smile is done by an attempt to bite the teeth together. With time it may be possible to learn how to use the new muscle to create a voluntary smile without the need to bite the teeth together.








 Episode one: A Fighting Chance
Episode one: A Fighting Chance
 Episode two: Smile
Episode two: Smile
 Episode three: Rogue Gene
Episode three: Rogue Gene
